Endoscopic Pituitary Adenoma Resection
What is Endoscopic Pituitary Surgery?
Endoscopic pituitary surgery, also called transsphenoidal endoscopic surgery, is the most common surgery used to remove pituitary tumors.
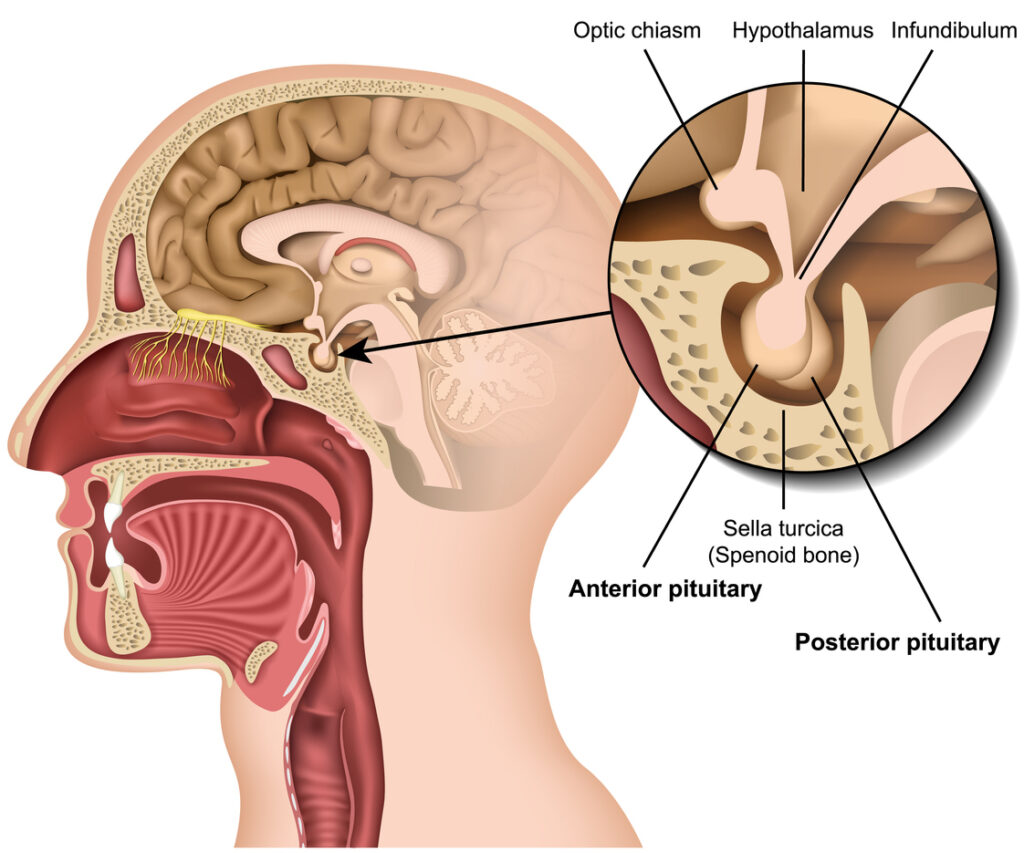
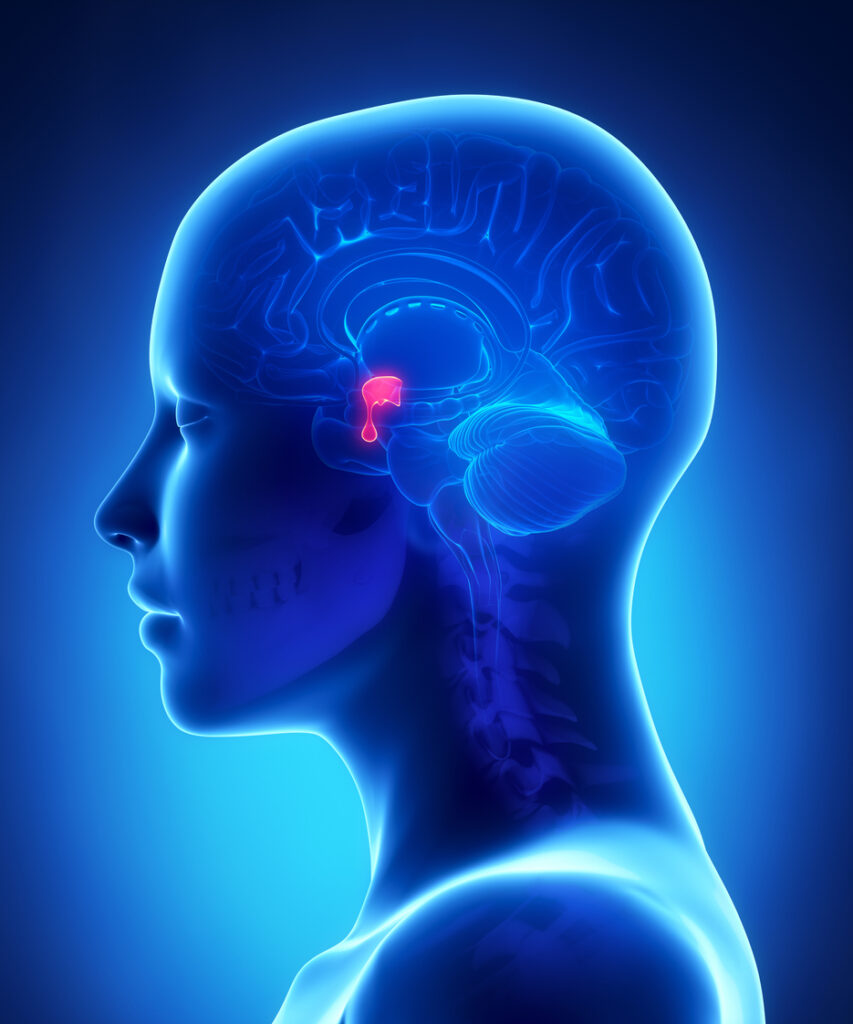
The pituitary gland is located at the bottom of your brain and above the inside of your nose. It is responsible for regulating most of your body’s hormones, the chemical messengers that travel through your blood.
Endoscopic pituitary surgery is done with an instrument called an endoscope. An endoscope is a thin, rigid tube that has a microscope, light, and camera built into it, and it’s usually inserted through the nose. The camera lets your surgeon watch on a television screen while inserting other special instruments through the scope to remove the tumor.
Reasons for Endoscopic Pituitary Surgery
- Pituitary Tumor – can cause abnormal hormone labs by either secreting hormones are by compressing the pituitary gland to cause gland dysfunction and producing hormonal irregularities. These are referred to hormone or non-hormone secreting tumors. This can produce problems with your thyroid hormone, growth hormone, steroids produced by your body, or other hormonal irregularities causing a variety of symptoms including tiredness, fatigue, heat/cold intolerance, excessive growth of certain body parts, and more.
- Loss of peripheral vision
- The pituitary gland sits under the optic chiasm, where the two optic nerve cross before going to your eyes.
- When a pituitary tumor grows it can cause compression of the optic chiasm and cause vision loss. Usually this vision loss is loss of bilateral peripheral vision.
- Surgery needs to be done in order to decompress the optic chiasm to prevent permanent vision loss.
- Excessive Growth
- If a pituitary tumor is found on a MRI, but is not causing symptoms, usually a repeat MRI is completed to make sure there has been no growth of the tumor.
- If the tumor exhibits growth on follow up MRI scans, surgery may be recommended.
Learn More About Pituitary Tumor Surgery
During Endoscopic Pituitary Surgery
The actual surgery may take a few hours. In many cases, an ear, nose, and throat specialist will work with a neurosurgeon in order to provide access to the tumor up through the nose, avoiding an incision. These steps may take place:
- The ear, nose, and throat surgeon usually places the endoscope through the nose. In some cases, the endoscope may be inserted through an incision under the upper lip.
The endoscope is advanced until the bony wall of the sphenoid sinus is found at the back of the nose. - The sphenoid sinus is opened and the scope is passed through to the back wall of the sinus.
- A small opening is made in the back wall of the sinus.
- Magnetic resonance imagining (MRI) may be used to make images of the pituitary area using a computer and magnets during the surgery to help guide the surgeons (navigation or stereotactic).
- When the pituitary area is entered, the neurosurgeon removes the pituitary tumor in small pieces.
- When all parts of the tumor that can be reached have been removed, the endoscope is removed. Some packing may be placed in the nose to complete the operation.
- If a CSF leak is encountered, sometimes fat from the abdomen is used or a flap from the patient’s septum is used to help recreate the barrier between the outside world and the brain, in order to repair the CSF leak.
Risks and Recovery
Risks of surgery include:
- CSF Rhinorrhea – CSF, or cerebrospinal fluid, is the fluid that surrounds the brain, and it may leak from the nose after surgery. In some cases, another surgery may be needed to repair this leak.
- Meningitis – This is a type of infection occurring in the membrane lining the brain and spinal cord that can occur after surgery. It is more common if the CSF leaks.
- Damage to normal parts of the pituitary gland – Damage to areas of the pituitary that secrete hormones may require hormone replacement after surgery.
- Diabetes insipidus – Damage to a part of the pituitary gland that helps control urination may lead to frequent urination and thirst.
- Severe bleeding – Heavy and persistent bleeding into the brain or from the nose may occur if a large blood vessel is damaged during surgery.
- Visual problems – The nerves that supply vision are close to the area of the pituitary gland and can be damaged.
After Surgery:
- You may need to stay in the hospital for a day or two.
- You will be encouraged to get out of bed and walk as soon as you are able.
- While in the hospital, you will be asked to help your nurses keep track of the amount of fluids you drink and your urine output to evaluate pituitary function.
Aftercare at home may include:
- Pain medication – to control headaches, the most common complaint after surgery
- Restricted activities – no lifting or straining until cleared by your surgeons
- Follow-up visits with your endocrinologist and surgeons
- Repeat MRI – to assess the extent of resection
- Visual testing – formally assess improvement of visual deficit
Schedule an appointment
- Contact Us
Ready to learn more? Contact us today to get started.
Make an Appointment
New & Existing Patients: Request An Appointment
New and existing patients may request an appointment by filling out the form below. Someone from our team will be contacting you to schedule an appointment time.